The details on identifying diverticulitis
/
The details on identifying diverticulitis
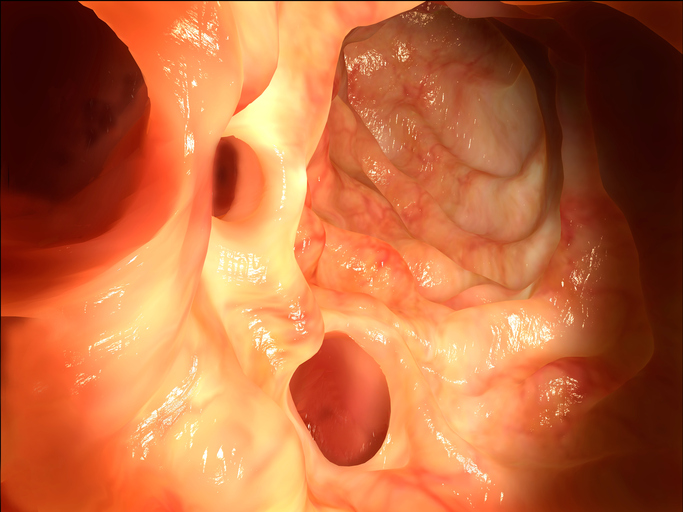
Diverticulosis is a condition in which small, bulging pouches (diverticula) form inside the lower part of the intestine, usually along weak spots in the wall of the colon. These pouches push outward along the wall of the colon and are the problem associated with diverticular disease.
When the diverticula become irritated, swollen, or inflamed, this can lead to infection (diverticulitis) or may cause a blood vessel in a pouch to burst open and bleed. Most people will not be aware if they have any diverticula lining the colon if they have no symptoms such as an infection or bleeding. This then is referred to as diverticulosis. For those individuals without symptoms, one way they may discover they have diverticulosis is when a colonoscopy is performed. Other people with diverticulosis may experience the following:
· Cramping or pain in the lower abdomen – the area between the chest and hips
· bloating
People susceptible to diverticular disease
Diverticulosis is more common as we age, particularly in people older than age 50. Even though seen most frequently in older adults, it is becoming more common in people younger than age 50 with most of them being men.
What are the symptoms of diverticulitis
The good news is less than 5 percent of people with diverticulosis will have diverticulitis. But it is still important to know the symptoms as there are many symptoms associated with diverticulitis. Diverticulitis means there is an infection in the pouches usually resulting in pain most common in the lower left side of the abdomen. Here are the symptoms of diverticulitis:
· Usually severe pain that comes on suddenly but can also be mild and worsen over several days
· Fevers and chills
· Nausea or vomiting
· A change in bowel habits – constipation or diarrhea
· Diverticular bleeding which can also lead to weakness, dizziness, and abdominal cramping
Diagnosing and treating diverticular disease
If diverticular disease is suspected, a healthcare provider may schedule one or more of the following tests: blood test, computerized tomography (CT) scan, lower gastrointestinal (GI) series, or a colonscopy.
Treating diverticular disease often includes recommending a high-fiber diet or fiber supplements, medications, and possibly probiotics.
Dodging diverticulosis and diverticulitis
There are several strategies a person can take to avoid diverticular disease. It is usually recommended to increase fiber even though some scientists have failed to find a link with eating a low fiber intake. Even so, there is some evidence a high fiber diet can help protect against diverticular complications. Here are steps to take dodging diverticulosis:
· Eat a high fiber (25-38 grams daily) diet rich in vegetables, fruit, and whole grains.
· Exercise regularly.
· Drink plenty of water – at least 6-8 cups a day or until urine is very pale looking.
· Maintain a healthy weight. Individuals with a body mass index of 30 or higher are at a greater risk of developing diverticulosis.
· Studies have linked nonsteroidal anti-inflammatory drugs (NSAIDS), such as ibuprofen, to increasing diverticulitis. Anyone with a history of diverticulitis should avoid non-aspirin NSAIDS.
· Adequate vitamin D might help reduce risk of diverticulitis. Top food sources of vitamin D are salmon, fortified milk, and eggs.
· It used to be thought eating nuts, seeds, and popcorn might lodge in diverticula. But a 2008 study following 50,000 men for 20 years found men who ate more nuts and popcorn were less likely to develop diverticular complications than those who ate very little of these foods.