Valley Fever: The Fungus Among Us
/If you live in the Southwest and think you “just have the flu,” you may want to think again. Valley fever, also called coccidioidomycosis, is an infection caused by the fungus Coccidioides, and its symptoms are almost identical to those of influenza.
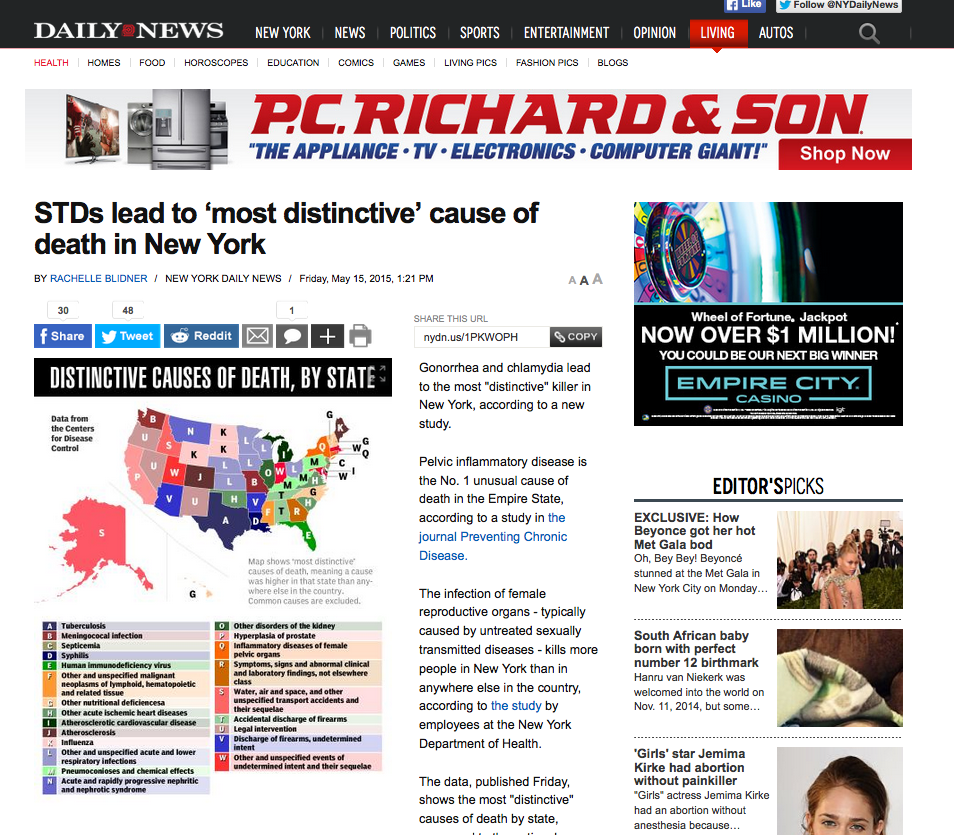
People can get Valley fever by breathing in the microscopic fungal spores from the air, although most people who breathe in the spores do not get sick. The fungus that causes Valley fever lives in soil and dust in Arizona, California, Nevada, New Mexico, Utah, Texas and parts of Mexico, Central America, and South America. The spores are extremely small and can be carried hundreds of miles by the wind. Once inside the lungs, the spores reproduce, perpetuating the cycle of the disease.
When symptoms of Valley fever do occur, they appear one to three weeks after exposure, and may include:
- Fever
- Cough
- Chest pain
- Chills
- Night sweats
- Headache
- Fatigue
- Joint aches
- Red, spotty rash
You won't mistake that rash for influenza. It is made up of painful red bumps that may later turn brown. The rash mainly appears on your lower legs, but sometimes on your chest, arms and back. Others may have a raised red rash with blisters or eruptions that look like pimples.
If you have contracted Valley fever but are asymptomatic, it may turn up as part of a routine blood test or chest X-ray.
Mild cases of Valley fever can resolve on their own, but it often progresses to something much more severe from which it can take months to recover, with fatigue and joint aches lasting even longer. How long you suffer depends upon your general health at the time you inhaled the spores, and how many spores you actually took in. In people with weakened immune systems, a chronic form of Valley fever can develop, with symptoms that can include:
- Low-grade fever
- Weight loss
- Cough
- Chest pain
- Blood-tinged sputum
- Nodules in the lungs
Valley fever is very difficult to diagnose, and is really only detectable via a sputum smear or blood test.
Treatment – even in many extreme cases – is usually only bed rest and fluids. In some cases your doctor may prescribe anti-fungal medications, but these can have notoriously onerous side effects. And although these anti-fungal meds can control the fungus, they may not destroy it, allowing relapses to occur.
Sources: Mayo Clinic