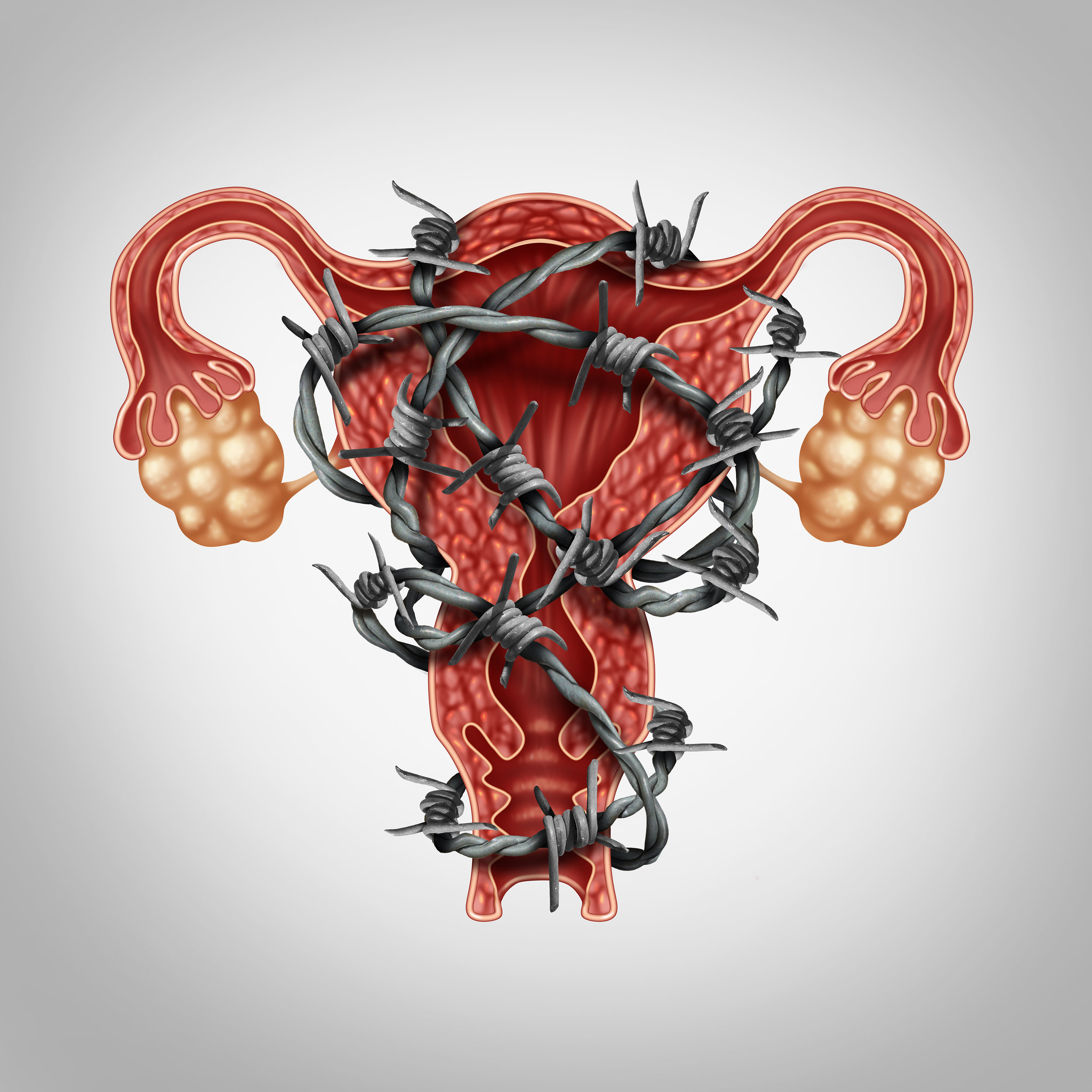
Understanding Endometriosis
/More than just a painful woman's disease – and it certainly is that! – endometriosis affects 1 in 10 women of reproductive age and raises the level of depression of the chronically afflicted by 15 to 20 percent. According to the New England Journal of Medicine, it is one of the top three causes of female infertility and, although treatable, remains the least treated.
What's it all about?
As unlikely as it sounds, endometriosis occurs when the tissue that normally lines the inside of your uterus — the endometrium — grows outside your uterus. The disease typically involves your fallopian tubes, ovaries, and the tissue lining your pelvis. In more cases, the tissue may spread beyond your pelvic organs.
Doctors still don't know exactly what causes your endometrium to go rogue, but there are a few theories:
- It's an immune system disorder. Under normal circumstances your body would destroy any endometrial tissue that grows outside of the uterus, but due to an immunological fault, your body does not recognize the flaw.
- It's a result of “retrograde menstruation.” That's a condition wherein menses flows back through the fallopian tubes and into the pelvic cavity instead of out of the body. Doctors believe that endometrial cells in that blood can stick to the pelvic walls and surfaces of pelvic organs, where they grow and continue to thicken and bleed over the course of each menstrual cycle.
- It's a product of “induction theory.” Some biochemists believe that hormones or immune system agents have the ability to transform peritoneal cells – those that line the inner side of your abdomen – into endometrial cells.
- It is caused by embryonic cell transformation. Some scientists believe that estrogen and other such hormones may transform embryonic cells into endometrial cell implants during puberty.
Whatever the cause, it hurts. A lot. And that's really the primary symptom. The pain may occur during intercourse, menstruation, bowel movements or urination. Secondary symptoms include fatigue, bloating, constipation, diarrhea and particularly heavy periods.
After giving you a physical pelvic exam, your gynecologist may schedule ultrasound imaging, which is useful for identifying the cysts often associated with endometriosis.
Once diagnosed, your doctor will likely start you out on a regimen of over-the-counter painkillers. Should you reach the upper levels of recommended doses for these – and it is likely you will – your gynecologist may try hormone therapy. Hormone-based meds can slow down the growth of endometrial tissue growth and prevent new implants of the tissue from occurring.
Because endometriosis may render you effectively infertile, surgery might be necessary if you suffer from the disease and want to have children. The surgery may be performed via traditional abdominal surgery, or laparoscopically.