How to protect yourself from deadly strains of E. coli
/How to protect yourself from deadly strains of E. coli
It’s happened once again – just before Thanksgiving 2018, the Centers for Disease Control and Prevention (CDC) sent out a public warning to avoid eating romaine lettuce due to links of a multistate outbreak of a nasty strain of E. coli 0157:H7. Romaine lettuce was also to blame for an E. coli outbreak across the U.S. resulting in dozens of illnesses, hospitalizations, and five deaths between November 2017 and June 2018.
This time, all romaine – including the pre-chopped variety, whole heads, and hearts - were quickly removed from all grocery stores across the U.S. while consumers who had any type of romaine lettuce already in their home, were strongly advised to toss it out to avoid the dangerous foodborne illness. So far, at least 50 people across 11 U.S. states and Canada have developed E.coli infections and at least 13 individuals in the U.S. had to be hospitalized. One victim of the outbreak has developed a type of kidney failure called hemolytic uremic syndrome.
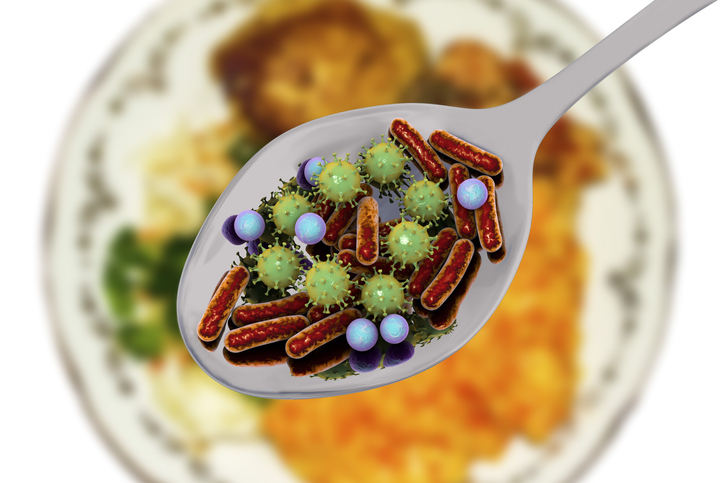
Understanding E. coli
E. coli or Escherichia coli, is a bacteria that normally lives in the intestines of healthy people and animals. There are more than 45 different strains of E. coli with most of them being harmless. But a few of them are particularly dangerous strains, such as E. coli O157:H7, which can cause severe abdominal cramps, bloody diarrhea and vomiting. E.coli O157:H7 produces a powerful toxin that damages the lining of the small intestine, which can cause bloody diarrhea. Even a small amount of E. coli can cause an infection – whether you ate slightly undercooked hamburger or swallowed a mouthful of contaminated pool water – in either case, you can be sickened by this bacteria.
There is always the possibility that any of us can be exposed to E. coli from contaminated water or food – especially raw vegetables and undercooked ground beef. Generally, healthy adults will recover from infection from E. coli O157:H7 within a week, but young children and older adults have a greater risk of developing a life-threatening form of kidney failure called hemolytic uremic syndrome, (HUS). One-third of children diagnosed with HUS do not recover completely, resulting in persistent renal failure and the need for long-term dialysis.
The symptoms of E. coli O157:H7 infection typically begins three or four days after exposure to the bacteria, but a person could become ill as soon as one day after to more than a week later. The signs and symptoms include the following:
· Diarrhea, which may range from mild and watery to severe and bloody
· Severe abdominal cramping, pain, or tenderness
· Nausea and vomiting, in some people
How does food and water become contaminated with E. coli?
There are several ways in which we can be infected or exposed to E. coli O157:H7 by eating or drinking contaminated food or water:
· Ground beef – When cattle are slaughtered and processed, E. coli bacteria in their intestines can get on the meat, if any of the bacteria happen to be E. coli O157:H7. If this particular strain of E. coli was present in the cow – not all cows will have this particular strain – ground beef would be especially prone to it. The reason is that ground beef or hamburger combines meat from many different animals, grinding them all together into ground beef, which could possibly increase the risk of contamination. This is why it is very important for anyone, but particularly children, the elderly, and anyone with a weakened immune system, should never eat undercooked ground beef.
· Unpasteurized milk – E. coli bacteria can be present on a cow’s udder or on milking equipment which can get into raw or unpasteurized milk.
· Fresh produce – Runoff from cattle farms can contaminate fields where fresh produce is grown. Certain vegetables, such as spinach and lettuce, are particularly vulnerable to this type of contamination.
· Contaminated water – Human and animal feces can pollute ground and surface water, including streams, rivers, lakes, and water used to irrigate crops. Although public water systems use chlorine, ultraviolet light or ozone to kill E. coli, some outbreaks have been linked to contaminated municipal water supplies.
Private wells are a greater cause for concern since they do not have any disinfecting system. Rural water supplies are the most likely to be contaminated. There have been cases of people swimming in pools or lakes contaminated with feces who have been infected with E. coli.
How to protect yourself from an E. coli infection
Fortunately, there are several steps you can take to safeguard and greatly reduce the chance of ever being infected with E. coli O157:H7. Practicing food safety is a must for everyone. Never assume that all food is automatically safe to eat. Here is how you can be assured to significantly protect yourself and others from experiencing food poisoning:
· Cook hamburgers until they are 160 degrees Fahrenheit – Hamburgers should always be well-done, with no pink showing anywhere in the meat. The juices should also be clear and not bloody looking. However, color is not a reliable indicator of whether the meat is cooked thoroughly or not – especially if grilled as the meat can brown before it’s completely cooked. That’s why it’s important to use a meat thermometer to ensure that meat is heated to at least 160 degrees F at its thickest point. If you are served undercooked hamburger or other ground beef product in a restaurant, send it back for further cooking.
· Only drink pasteurized milk, juice and cider
· Wash raw produce thoroughly – Washing produce won’t necessarily get rid of all E. coli – especially in leafy greens, which provide many spots for the bacteria to attach themselves to. Careful rinsing can remove dirt and reduce the amount of bacteria that may be clinging to the produce.
· Avoid cross-contamination:
· Wash utensils – use hot soapy water on knives, countertops, and cutting boards before and after they come into contact with fresh produce or raw meat. Use separate cutting boards for produce and raw meats.
· Keep raw foods separate from raw meat, poultry or fish. Never put cooked hamburgers on the same plate you used for raw hamburger patties.
· Wash your hands – Always wash hands before preparing or eating food, using the toilet, changing a diaper, or after contact with animals, animal feces, and animal environments. Make sure that children also wash their hands before eating, using the toilet, or after contact with animals.
· Use caution when swimming – Avoid swallowing lake, pool water, or backyard “kiddie” pools while swimming. Anyone with a diarrheal illness should avoid swimming in public pools or lakes, sharing baths with others, and preparing food for others.